Infections
Summary
Infections are caused by invasions of microorganisms such as bacteria, viruses, and parasites that are not normally present in the body. Since the first observation from the 19th century that infectious agents can play a role in the development of cancer, continuous research has been conducted to understand the viral etiology of cancer. Directories such as the GLOBOCAN 2018 database estimated that 2.2 million cancer cases were attributed to infection, where researchers stated that Helicobacter pylori (H. pylori), Human papillomavirus (HPV), Hepatitis B and Hepatitis C virus were the primary causes of these cancers [1]. The most common viral infections that can develop cancer are HPV, Hepatitis B and C, and Epstein-Barr virus (EBV) [2]. Apart from these viral infections, there are other pathogens such as Helicobacter pylori (H. pylori), Haemophilus influenzae, and Escherichia coli that have also been linked to cancer. With advancing technology and breakthroughs in research, more information on cancer-related mutations and viruses is being evaluated to determine the best treatments.

Sindi Castillo
Undergraduate from Lamar University
As the understanding of cancer continues to be researched, significant developments give way that direct therapies and treatments, such as the implication of single-molecule targeted therapy, the use of checkpoint inhibitors, and that of of the STING (stimulator of interferon genes), might be a future direction in tackling cancer with more accuracy.
Our current medical climate includes growing concern toward the COVID-19 pandemic. As the COVID-19 virus continues to evolve and spread throughout the population, its future effects on those infected remain uncertain. Like any mutation, a better understanding of the viral mechanisms is needed to determine its underlying effects. As previously noted, several infections can lead to cancer after the production of tumorigenesis, inflammation, or excessive exposure to carcinogens. While current studies give way to the relationship between infections and cancer, more research needs to be conducted to comprehend the nature and mechanisms of this correlation.
References
- de Martel, Catherine, et al. “Global Burden of Cancer Attributable to Infections in 2018: A Worldwide Incidence Analysis.” Lancet Global Health 8 (2019): 180-190. https://doi.org/10.1016/S2214-109X(19)30488-7
- Tashiro H, Brenner MK. “Immunotherapy against cancer-related viruses”. Cell Res. 2017;27(1):59-73. doi:10.1038/cr.2016.153
Full Article
Cancer is the uncontrolled growth of cells in any location of the body that results in a malignant tumor. The growth of cancer may be caused by a variety of factors, including bacterial or viral infection, genetic mutations, lifestyle choices, or other environmental factors. Infections are caused by invasions of microorganisms such as bacteria, viruses, and parasites that are not normally present in the body. While current studies give way to the relationship between infections and cancer, more research needs to be conducted to comprehend the nature and mechanisms of this correlation.
Bacterial and viral infections have been correlated as a cause of cancer (refer to Table 1). The GLOBOCAN 2018 database estimated that 2.2 million cancer cases were attributed to infection, where researchers stated that Helicobacter pylori (H. pylori), Human papillomavirus (HPV), hepatitis B and hepatitis C virus were the primary causes of these cancers [1]. While cancer is not contagious in the sense that it is transmitted from one patient to another through close proximity, studies reveal that several cancers worldwide have infectious etiology [1, 2]. Although this study was taken globally, it does include underdeveloped countries that are more affected by viruses and other infections. This can make the study seem less accurate, but there is consistent research throughout history to deem infections as a cause of cancer. The observation that infectious agents can play a role in the development of cancer dates back to the 19th century. In 1842, physician Domenico Rigoni-Stern concluded that the development of cervical cancer is related to sexual contact after analyzing death certificates and the relationship between the risks of breast and cervical cancer of nuns, married women, and sex workers [2]. Due to the lack of knowledge in viruses at the time, it was not until the 20th century that a tumor-inducing virus was discovered. In cancer-causing viruses, oncogenes were first identified and their ability to induce a transformation in cells. Before this time, oncogenic viruses had no correlation to cancer and was instead an experiment set forth towards animal models. The viral etiology of cancer was first demonstrated in 1911 by Peyton Rous who injected healthy chickens with the extraction of tumor tissue from a chicken sarcoma and noted that it could induce tumors [3]. The discovery of the first human tumor virus as the Epstein-Barr virus in 1964 came as a result of Denis Burkitt’s seminal work of identifying a common childhood tumor in equatorial Africa yet, at the time, was unknown in the West [4]. This work was led by Anthony Epstein and his team who identified herpesvirus-like particles in cultured tumor cells derived from what is now known as Burkitt’s Lymphoma (BL). Since this discovery, further research has been done to establish other pathogens as human cancer viruses and to gain a better understanding of its mechanisms.
Each of the potential pathogens in Table 1. has been noted as human infections that promote related cancers. The most common viral infections that can develop cancer are HPV, Hepatitis B and C, and Epstein-Barr virus (EBV) [5]. Bacterial infections like Helicobacter pylori (H. pylori) can cause ulcers and ultimately gastric cancer. H. pylori has an oncoprotein known as CagA that alters epithelial cells and disrupts assembly and signaling that occurs in the gastric mucosa [6]. This protein can reduce epithelial cell apoptosis (programmed cell death) by interfering with tumor suppressors and can promote cancer development. Overall, infection with H. pylori is extremely common and the risk of developing gastric cancer is dependent on the response of the H. pylori strain and other factors that include the host genotype, and environmental factors, such as diet. Another bacterial infection, Haemophilus influenzae, commonly leads to respiratory infection and inflammation. These conditions may escalate into pneumonia and Chronic Obstructive Pulmonary Disease (COPD), which is a risk factor for lung cancer [7]. Escherichia coli, a bacteria most commonly located in the intestines, has been implicated in the causation of cancer, as well. It has been shown that a diet rich in fat and red meat is deleterious to physical health. This “Western diet” causes changes to the bacteria present in the intestines. The resulting imbalances between bacterial communities in the gut, such as E. coli, contribute to inflammation and metastasis of colorectal cancer [8]. The most studied cancer-causing viruses include Epstein Barrvirus (EBV), Human papillomavirus (HPV), Hepatitis B virus (HBV), and Hepatitis C virus (HCV). EBV is an episome, meaning the virus integrates itself into the host cell’s DNA in order to reproduce. A study by Chen et al. detected the presence of EBV in tumor cells of gastric cancer patients, as well as patients with Non-Hodgkin’s lymphoma [9]. While most HPV infections clear up on their own, there is a risk that a prolonged infection with this virus can lead to the development of cervical cancer. This type of infection has been identified through viral DNA sequences in the tumor tissues and is a result of a long-lasting infection that can lead to the conversion of normal cells in the surface of the cervix to turn into cancerous cells [9]. The human HBC virus has been shown to commonly integrate into the genomes of liver tumor cells [9]. A viral integration occurs when a virus inserts its DNA or cDNA into its cell’s host genome. When this occurs, the HBC genes can contribute to tumorigenesis in the liver if the genes are expressed as host-virus fusion transcripts. Lastly, people infected with the HCV virus have been studied to be at an increased risk of developing certain lymphomas, including Non-Hodgkin’s lymphoma [10]. This virus can trigger B-cells and promote favorable conditions for B lymphocyte proliferation that can produce Non-Hodgkin’s lymphoma. An infection will not always cause cancer, but understanding the development of it can either help prevent one from progressing or aid in understanding its correlation to cancer.
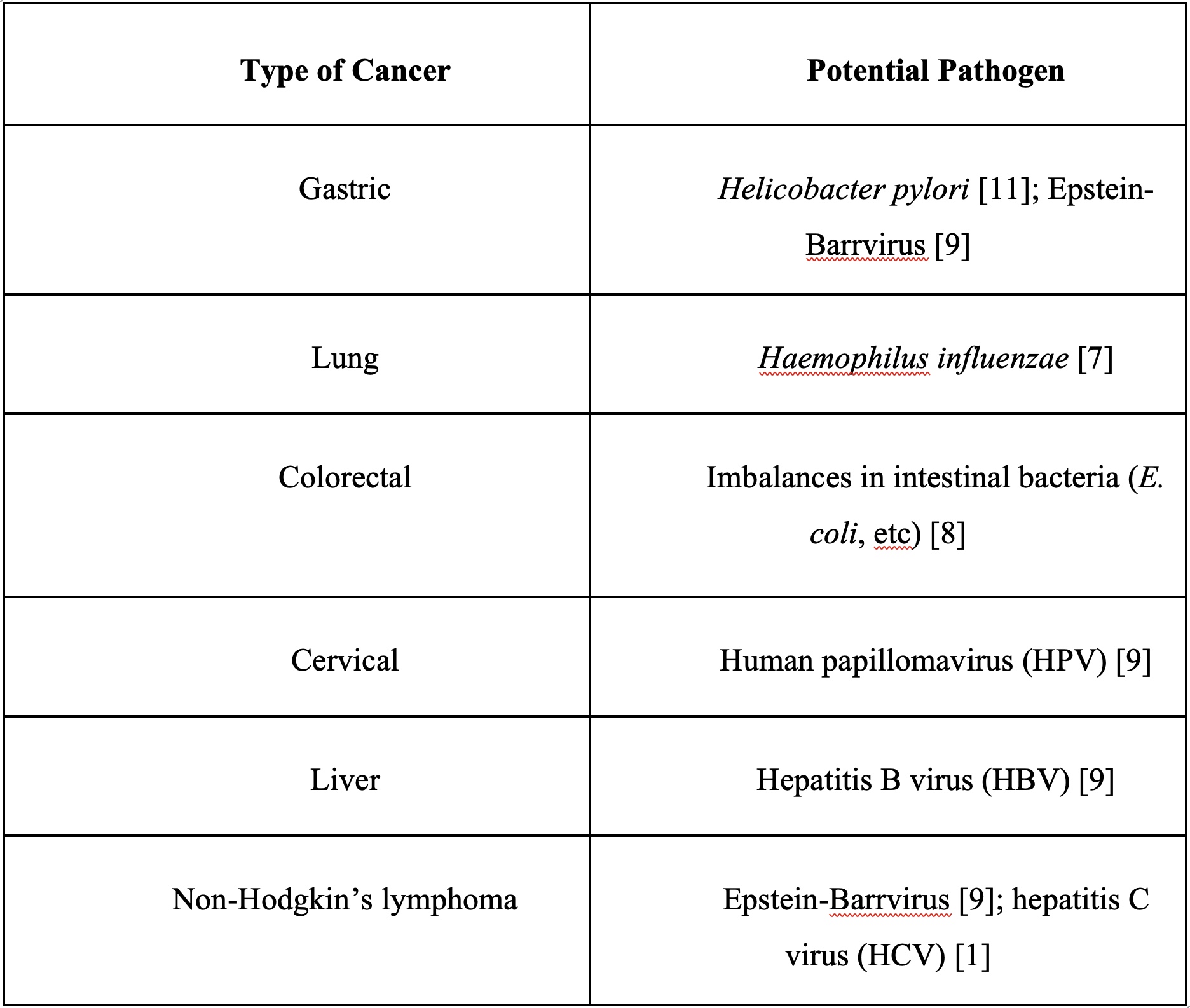
Table 1. Common Cancers and Associated Pathogens: This table outlines various potential pathogens and related cancers.
There is a perspective that the root cause of many cancers is due to microbial and parasitic invasion in the organs or colon. The theory states that this invasion weakens the immune system directly and indirectly through the excretion of mycotoxins and intercepting cells from receiving glucose. This is due to the microbes weakening the immune system to keep it from fighting back and killing them. The immune system is then too weak and cannot kill cancer cells so they continue to grow out of control. This theory states that the microbe itself is what is causing cancer, but in order for cancer to develop, the microbe needs to go through other cancer hallmarks like mutations and chronic inflammation. This perspective is not entirely correct as it does not give any statement that the microbe has to go through any further stage to develop cancer. Conversely, current research disproves this perspective and does not support microbial and parasite invasion to be the “root” cause of many cancers. In reality, researchers have found that most cancers occur through processes that alter DNA in cells [12]. While microbial invasion is not the one event directly causing cancer, infections like the ones previously explained can set the stage for cancer development. The distinction is that infections can promote tumorigenesis through instances of DNA errors and other factors. In the case of some viruses, they have the capability to adapt to new hosts and environments. They do so by being able to mutate,which usually results in a higher genetic variability [13]. During the mutation process, there is always the risk of DNA copying errors that can eventually lead to the development of cancer.
Finally, cancer-related infections are important to understand due to the rising number of cancer diagnoses. Cancer is the second leading cause of death globally and is on track to surpass ischemic heart disease and stroke as number one by 2060 [14]. With advancing technology and breakthroughs in research, more information on cancer-related mutations and viruses is being evaluated to determine the best treatments. There is increasing interest in the implication of single-molecule targeted therapy, which shows evidence of increased response and survival rates compared to other treatments involving chemotherapy and radiation [15]. A significant recent development is the discovery of immune checkpoint inhibitors. These inhibitors allow immune cells in our bodies to recognize and destroy cancer cells [16]. Another breakthrough is the discovery of the STING (stimulator of interferon genes), which has allowed for the development of immunization regimes and other therapies to treat cancers with more accuracy [17]. STING signaling has been noted to protect cells from various pathogens and even against the development of cancer by promoting antitumor immune responses. As the understanding of cancer continues to be researched, significant developments give way that direct therapies and treatments might be a future direction in tackling cancer.
Infections are a result of an invasion of a microorganism in one’s body that can cause disease. While not all infections lead to cancer, some have been noted to promote tumorigenesis, inflammation, or other factors that can result in a malignant tumor. Our current medical climate includes growing concern regarding the COVID-19 pandemic. Considering that cancer patients already have weakened immune systems, it is imperative that all precautions are taken to prevent infection by SARS-CoV-2, which is the virus that causes COVID-19. It is recommended that cancer patients consult the guidelines set by the World Health Organization and the Centers for Disease Control and Prevention, and consult their cancer care facility for any changes to treatment. As the COVID-19 virus continues to evolve and spread throughout the population, its future effects on those infected remain uncertain. Like any mutation, a better understanding of the viral mechanisms is needed to determine its underlying effects.
References
- de Martel, Catherine, et al. “Global Burden of Cancer Attributable to Infections in 2018: A Worldwide Incidence Analysis.” Lancet Global Health 8 (2019): 180-190. https://doi.org/10.1016/S2214-109X(19)30488-7
- Chang Y, Moore PS, Weiss RA. Human oncogenic viruses: nature and discovery. Philos Trans R Soc Lond B Biol Sci. 2017;372(1732):20160264. doi:10.1098/rstb.2016.0264
- Lunn RM, Jahnke GD, Rabkin CS. Tumour virus epidemiology. Philos Trans R Soc Lond B Biol Sci. 2017;372(1732):20160266. doi:10.1098/rstb.2016.0266
- Shannon-Lowe C, Rickinson A. The Global Landscape of EBV-Associated Tumors. Front Oncol. 2019;9:713. Published 2019 Aug 6. doi:10.3389/fonc.2019.00713
- Tashiro H, Brenner MK. “Immunotherapy against cancer-related viruses”. Cell Res. 2017;27(1):59-73. doi:10.1038/cr.2016.153
- Amieva M, Peek RM Jr. Pathobiology of Helicobacter pylori-Induced Gastric Cancer. Gastroenterology. 2016;150(1):64-78. doi:10.1053/j.gastro.2015.09.004
- Bose, Mukulika and Pinku Mukherjee. “Microbe-MUC1 Crosstalk in Cancer-Associated Infections.” Trends in Molecular Medicine 26 (2020): 324-336. doi.org/10.1016/j.molmed.2019.10.003
- Liu, Chen-Jian, et al. “Intestinal bacteria detected in cancer and adjacent tissue from patients with colorectal cancer.” Oncology Letters 17 (2019): 1115-1127. doi:10.3892/ol.2018.9714
- Chen, Xun, et al. “A virome-wide clonal integration analysis platform for discovering cancer viral etiology.” Genome Research 29 (2020): 819-830. doi:10.1101/gr.242529.118
- Jette, Nicholas R., et al. “ATM-Deficient Cancers Provide New Opportunities for Precision Oncology.” Cancers 12 (2020): 1-13. doi:10.3390/cancers12030687
- Zhang, Xiao-Ying, et al. “From inflammation to gastric cancer: Role of Helicobacter Pylori (Review).” Oncology Letters 13 (2017): 543-548. doi:10.3892/ol.2016.5506
- Mertz, T. M., Harcy, Victoria, and Roberts, S.A. 2017. Risks at the DNA Replication Fork: Effects upon Carcinogenesis and Tumor Heterogeneity. Genes (Basel) 8: 46.
- Sanjuán R, Domingo-Calap P. Mechanisms of viral mutation. Cell Mol Life Sci. 2016;73(23):4433-4448. doi:10.1007/s00018-016-2299-6
- Mattiuzzi, Camila and Giuseppe Lippi. “Current Cancer Epidemiology.” Journal of Epidemiology and Global Health 9 (2019): 217-222. https://doi.org/10.2991/jegh.k.191008.001
- Peng, Miao, et al. “Neoantigen Vaccine: An Emerging Tumor Immunotherapy.” Molecular Cancer 18 (2019): 1-14. https://doi.org/10.1186/s12943-019-1055-6
- Zaidi, Neeha and Elizabeth M Jaffee. “Immunotherapy Transforms Cancer Treatment.” The Journal of Clinical Investigation 129 (2019): 46-47. https://doi.org/10.1172/JCI126046
- Barber GN. STING: infection, inflammation and cancer. Nat Rev Immunol. 2015;15(12):760-770. doi:10.1038/nri3921