What is COVID-19?

Where did COVID-19 come from?
Early investigation suggests that the first cases of COVID-19 were directly related to an animal market in Wuhan, China. The origin of the virus is proposed to come from bats due the sharing of 96% of nucleotide identity between the novel coronavirus, and a known bat coronavirus. The first cases of coronavirus were reported between December 18 and December 29, 2019 [2]. At this point there was no reason to believe that the virus would transmit from human to human because there were no reports of healthcare workers becoming infected [1]. However, the first case of human to human transmission was reported on January 30, 2020 [2]. Within 3 months of the initial report there were 80,555 confirmed cases in China, and 17,821 confirmed cases in 90 countries outside of china. By March 11, 2020 COVID-19 had spread to at least 114 countries and was therefore declared a pandemic by the World Health Organization (WHO) [2].
How does COVID-19 spread?
There are several ways through which COVID-19 can spread. This includes contact and droplet, fomite, and airborne transmission. Contact and droplet transmission was the first known way of transmission of COVID-19 [1]. This type of transmission occurs through direct, indirect or close contact with droplets of an infected person [3]. What this means is that when an infected person, without face coverings, sneezes, coughs, or talks they expel droplets of saliva and other respiratory secretions, which can then come into contact with a healthy person, thus spreading the infection from person to person directly. However, these droplets can land on objects and contaminate them. Then, if the object is not sanitized properly the next person who touches the object can become infected also, this is called fomite transmission. Studies have shown that COVID-19 can remain viable on surfaces such as stainless steel, plastic, glass, and cardboard, for several hours [9]. This increases the risk of spread through fomite transmission. Lastly, airborne transmission while not common outside of the health care setting is still possible. Airborne transmission happens when droplets disintegrate and become aerosols. These aerosols can remain in the air for long distances and time (3-16 hours) which increases the risk of infection [3].
What are the known symptoms of COVID-19?
Symptoms of COVID-19 usually appear 2-14 days after exposure and may include [4]:
- Fever
- Chills
- Cough
- Shortness of breath
- Fatigue
- Muscle or body aches
- Headache
- New loss of taste or smell
- Sore throat
- Congestion
- Nausea and vomiting
- Diarrhea
It is also important to note that the World Health Organization stated that about 80% of COVID-19 cases are mild or asymptomatic [5].
Who is most at risk of contracting COVID-19?
Although everyone is at risk of getting COVID-19, there are two main groups of people that have a higher risk of becoming severely ill. First are older adults, because the risk of contracting COVID-19 increases with age. Likewise, people with underlying conditions such as: cancer, type 2 diabetes, and sickle cell among many others [6]. It is especially important that people that are most at risk follow all safety protocols that have been put in place to prevent the spread of the virus. This is because the immune system of these people puts them at risk for more complications.
What are the available testing options?
There are two ways of testing for COVID-19, viral and antibody tests [6]. Viral tests determine if you have COVID-19 at the time of the test. This consists of testing a sample from your respiratory system collected through nasal swabbing. The virus test is utilized to see if your respiratory system contains the virus. The second kind of test is antibody tests. These can tell you if you previously had COVID-19. This test checks your blood for antibodies, which are proteins that help fight off infections. The reason this test can only tell you if you had the virus in the past is because it normally takes the body 1 to 3 weeks after infection for antibodies to form [6]. If you have been exposed, it is important that you get tested to prevent the further spread of COVID-19.
Safety measures
To prevent the spread of COVID-19 it is recommended that you [7]:
- Wash and sanitize hands often
- Social distance (at least 6 feet)
- Wear mask
- Cover coughs and sneezes
- Clean and disinfect surfaces often
Recently the use of masks has been a matter of debate. One popular argument against the use of masks, is that masks limit oxygen intake. However, this claim has absolutely no scientific or clinical evidence behind it [8]. Another argument that people who are against the use of masks have is that masks are not effective so there is no point in wearing one, some going so far to say wearing masks is a ploy to force compliance. According to a study done at Lamar University, it was found that anything from medical grade masks, N-95s, to homemade cloth masks, can help stop bacteria from spreading. So long as the mask can keep droplets of moisture from leaving your mouth and nose, it can help prevent the spread of COVID – 19. While they understand that COVID – 19 is a virus and not bacteria, the fact that the masks can stop bacteria shows that they are strong protectors against the spread of other microbes, such as viruses. As previously mentioned, people with COVID-19 can be relatively asymptomatic, and still be able to transmit the virus to others. While masks are not 100% effective in protecting the wearer, they are effective in protecting those around them [8]. Therefore, if everyone wore a mask, we would all be better protected from the virus.
How Viruses Mutate?
In order to have a better understanding of COVID-19, it is important to understand it in the sense of a virus such as what it is and how it works. COVID-19 is a virus. Viruses are essentially genetic material wrapped in a protective envelope of fats and proteins [9]. Although viruses are not considered to be living things, they do have a life cycle. The life cycle of a virus consists of them finding a living host, infecting them, and then being transmitted to a new host [10]. This cycle is vital to the success of a virus because the living host has the machinery that viruses do not have, but need to reproduce [11]. In order to understand the spread of COVID-19, we need to understand the lifecycle of a virus and how they mutate.
Since all viruses require a host in order to reproduce, they must come into contact with a viable host before they can begin multiplying. Not all living things can be a host for every virus. The host needs to have proteins on the outside of their cells that are compatible to those on the outside of the virus. These proteins are the way viruses interact with their host. They work like a lock and key. The proteins on the host’s cells are the lock, and the proteins on the virus are the key. Without the right key, the virus cannot enter its genetic material into the cells of the host. There are also other barriers viruses must avoid in order to insert their genetic material into the host cells, namely the antibodies in the blood of the host that bind to the virus’s proteins and block them from binding with and inserting their genetic information into their target cells. Kind of like if you put a thimble on the end of a key. The key would not be able to fit in the lock anymore [10, 11].
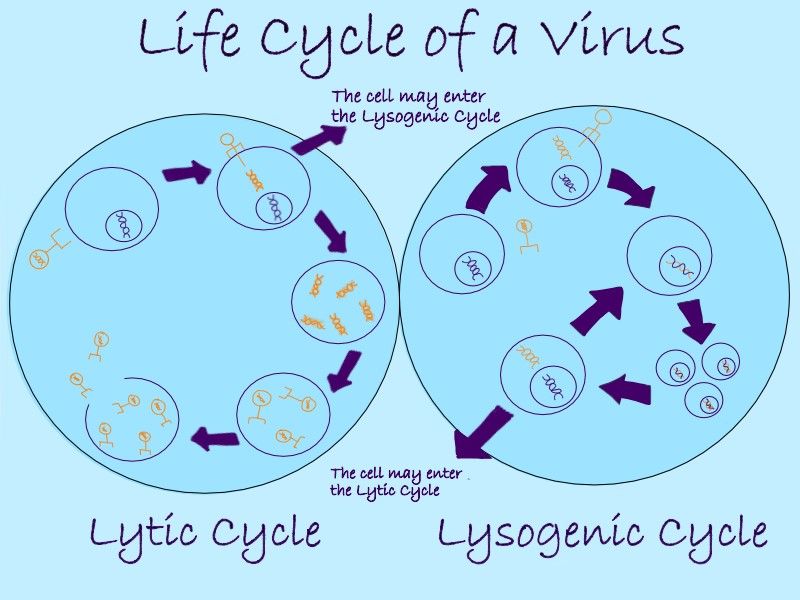
Once the virus has successfully entered its genetic material into the host, it is considered to have infected the host [10]. From here there are two ways that the virus can use the cell to replicate its genetic information. One way is to have the cell replicate the virus over and over again until it creates so many copies of the virus that the cell can no longer hold anymore and the cell bursts, or lyses. This releases the copied viruses, making them free to infect other cells and hosts [11]. This is called the lytic cycle. The second way a virus can use a host’s cells to replicate its genetic information is have its genetic information integrate with the host’s. This way when the host replicates its genes through its normal life processes, the virus’s genes are replicated as well. This process is known as the lysogenic cycle [11]. Some viruses are capable of shifting between the two different cycles such as HIV. The switch is generally caused by triggers in the host’s body or environment [11].
I think for right now I am just going to leave my citations highlighted with the name of their respective refs. Once we reorder the refs, I will put in the right numbers.
COVID – 19 uses the lytic cycle when it infects people [12]. The virus has special proteins that bind with cells in the lungs. Once it has infected the lungs, it has the cells of the lungs replicate the virus until the cells burst. This leaves permanent scarring in the lungs of many COVID – 19 patients [12]. The use of the lytic cycle for replication also means that the virus is replicated a lot in a very short period of time. This rapid replication leaves room for a lot of random error in the genetic material of the genes [13]. These random errors create mutations in the virus that can change the virus in many different ways [13]. Some of these genetic changes can help it jump species like it did in China at the very start of the pandemic [10]. Some can lead to a completely different strain, similar to how there are multiple strains of the flu virus, which can eventually become immune to certain vaccines [13, 14, 15].
While coronaviruses like the COVID – 19 have been shown to mutate quickly, these mutations can be both helpful and detrimental to the viruses, and the mutations are passed on in a survival of the fittest style [15, 13]. In conditions where a virus is thriving, most mutations do not serve to help the virus, and die off since they do not prove to be more useful to the virus’s survival. This seems to be the case with COVID – 19. While that does not rule out all mutations for the future, given how easily the virus is transmitted and how well it fares in affected hosts, it is not likely to mutate dramatically [13]. This makes hopes for developing a vaccine for COVID – 19 a little more attainable since there shouldn’t be huge shifts to deal with from now until the first vaccines [13].
Another measure that helps to stop further mutation is taking the precautions outlined above under safety measures. These measures, outlined by various groups, help to reduce the chances of the virus coming into contact with new hosts. Without a new host, the virus cannot replicate, decreasing the chances of mutation. This helps increase hope of a vaccine and end the pandemic.
Looking into treatments and vaccines, it is important to note the difference and how they can be used to combat COVID – 19. In regards to viruses, vaccines are used to prevent infection by a virus whereas treatments are meant to ease the symptoms of an infected individual [16]. Since viruses are not living organisms, you can’t administer antibiotics to kill them like you would bacterial or fungal infections [11]. Instead you have to let the virus run its course. [11] This is why preparing your body for an attack with a vaccine is useful. Vaccines act as a sort of boot camp for your immune system so that it can build its arsenal of antibodies to fight enemies that resemble the vaccine [14]. Vaccines expose the body to a form of the virus that can not infect the individual. This exposure does more than just strengthening the immune system. It allows a person’s body to make antibodies that will be prepared to attack future invasions by the virus, without putting the person in jeopardy of catching the disease. Since each virus has a unique set of binding proteins, which is how the immune system identifies specific viruses to make and release antibodies, not being exposed to the virus through vaccination leaves a person without the specific antibodies to fight the virus when they are exposed to a kind that can infect them. This leaves the body unequipped to fight off the virus and stop infection as quickly as it would have, had the person been vaccinated. While there are cases in which the prepared antibodies are not able to completely stop all infection by the virus, having the vaccine helps to stop the infection from being worse than it would be without any preparation [14, 15]. There are some individuals who have said that vaccines can cause more detrimental side effects such as autism and death, but the connections to autism have not been able to be replicated in scientific studies and the number of deaths related to vaccines is much smaller, if existent, in comparison to those related to the viruses they are meant to help protect against [17].
How Does COVID-19 Affect Cancer Patients?
Cancer patients and those with a history of cancer are at higher risk of infection by SARS-CoV-19 due to their compromised immune systems. In addition to immunosuppression, factors that make cancer patients more susceptible to COVID-19 include frequent hospitalization, advanced age in many cases, and poor functionality [18]. Cancer patients also experience a higher incidence of “severe events” (death or ICU admission) which may be exacerbated by recent surgery or immunotherapy treatment [19]. Cancer care systems are experiencing many challenges as a result of the COVID-19 outbreak, including drug shortages, risks associated with interventional cancer diagnosis procedures, and maintenance of safety in outpatient facilities [20]. Top cancer care facilities like MD Anderson Cancer Center are taking the necessary precautions to ensure the safety of their patients [21]. Such measures include delay of surgical intervention, if possible, modification of antitumor therapies, restriction of visitors, drive-through medication services, and education regarding procedures recommended by the World Health Organization and the Centers for Disease Control and Prevention.
Developments regarding the coronavirus are being made every day. Many companies are already undergoing trials with experimental vaccines, circumventing animal testing to take the most efficient route possible. The development of an effective vaccine typically takes up to 20 years, first going through the identification of a candidate and then three trial phases [22]. There are both pros and cons to such an expedient pathway. By evading animal testing, companies save time and money and potentially avoid the delay of treatment [22]. While this could result in a solution quickly, we must also consider potential damages and setbacks. The lack of animal testing makes it difficult to predict the effect of a vaccine on humans. In addition, the use of animal testing allows us to observe the likelihood that the vaccine increases instances of infection and severe complications [22]. Some parties believe that bypassing animal trials is unethical, while others uphold that the risk is worth the possibility of a vaccine being viable. It should be pointed out, however, that animal studies do not always accurately predict how a drug will work in a human. It is difficult to say whether cancer patients will be viable candidates for vaccination, because the introduction of the virus via vaccine to a cancer patient’s weakened immune system may have detrimental consequences.
Some studies have utilized prescription antiviral drugs for the treatment of COVID-19, but their efficacy is inconclusive [23]. One regimen, in particular, has gained the attention of United States officials, calling for the use of hydroxychloroquine to battle the pandemic. The physician at the front line of this claim is Dr. Stella Immanuel, a doctor based in Houston, Texas, who has been both praised and criticized for her assertion that hydroxychloroquine is a cure for COVID-19. A viral video of Dr. Immanuel caused an uproar in the medical community. The following subsequent approval of hydroxychloroquine by the FDA caused a wide-spread shortage of the drug, depleting its availability to those who relied on the medicine for the treatment of autoimmune diseases [24]. Initial studies supporting the hydroxychloroquine argument have not been replicable, and are criticized as being inadequate in terms of sample size and statistically relevant findings [24]. The World Health Organization and Centers for Disease Control and Prevention have both denied the hydroxychloroquine “cure”, and the Food and Drug Administration recently revoked their approval.
The COVID-19 pandemic is a rising barrier for cancer research, due to the decrease in trial availability and deviation from the protocol for patient visits [20]. As the virus continues to spread, cancer research laboratories are turning their focus toward utilization of cancer drugs for the treatment of novel coronavirus [25]. The ethics of continuing research are a major concern, and the FDA has passed amendments for the management of cancer clinical trials during the pandemic. These amendments include keeping patients informed of alterations, assuring the safety of trial participants, maintaining good clinical practice, and facilitating open communication with drug developers. The most harrowing hurdle for cancer research during the outbreak is the decrease in funding from both government and non-profit sectors [25]. As more of the governmental research budget is allocated toward finding a coronavirus “cure”, cancer therapy trials and their results are taking the back burner. Donations from outside sources and further support for cancer research efforts will be pivotal to continuing progress.
References
- Park SE. Epidemiology, virology, and clinical features of severe acute respiratory syndrome -coronavirus-2 (SARS-CoV-2; Coronavirus Disease-19). Clin Exp Pediatr. 2020;63(4):119-124. doi:10.3345/cep.2020.00493
- Bulut C, Kato Y. Epidemiology of COVID-19. Turk J Med Sci. 2020;50(SI-1):563-570. Published 2020 Apr 21. doi:10.3906/sag-2004-172
- Transmission of SARS-CoV-2: implications for infection prevention precautions. (n.d.). Retrieved August 5, 2020, from Who.int website:
- https://www.who.int/news-room/commentaries/detail/transmission-of-sars-cov-2-implications-for-infection-prevention-precautions
- CDC. (2020, July 29). Coronavirus Disease 2019 (COVID-19) – Symptoms. Retrieved August 5, 2020, from Cdc.gov website: https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html
- Who.int.https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200306-sitrep-46-covid-19.pdf?sfvrsn=96b04adf_4#:~:text=For%20COVID%2D19%2C,infections%2C%20requiring%20ventilation. Accessed August 5, 2020.
- CDC. Coronavirus Disease 2019 (COVID-19). Cdc.gov. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/older-adults.html. Published August 1, 2020. Accessed August 6, 2020.
- CDC. Coronavirus Disease 2019 (COVID-19) – Prevention & Treatment. Cdc.gov. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html. Published July 31, 2020. Accessed August 6, 2020.
- From the frontlines: The truth about masks and COVID-19 | American Lung Association. Lung.org. https://www.lung.org/blog/covid-masks. Accessed August 6, 2020.
- What is a Virus? Breakthrough https://www.youtube.com/watch?v=kufvGibHWTM&t=6s
- How do viruses jump from animals to humans? – Ben Longdon https://www.youtube.com/watch?v=xjcsrU-ZmgY&t=153s
- Viruses (updated) https://www.youtube.com/watch?v=8FqlTslU22s
- The Coronavirus Explained & What You Should Do https://www.youtube.com/watch?v=BtN-goy9VOY&list=WL&index=6&t=0s
- How Viruses Like Corona Virus Mutate https://www.youtube.com/watch?v=WOVJ9XgYvac&t=1s
- How do you know if you have a virus? – Cella Wright https://www.youtube.com/watch?v=jEs9PzHc9ho
- Animation: Why the Flu Virus Changes and Mutates https://www.youtube.com/watch?v=R8c87p0xI9Q
- What Could Be The Fastest Way To End The Coronavirus Crisis? https://www.youtube.com/watch?v=aXW9cDN0IpY&t=10s
- The Side Effects of Vaccines-How High is the Risk https://youtu.be/zBkVCpbNnkU
- Shankar, Abhishek, et al. “Cancer Care Delivery Challenges Amidst Coronavirus Disease – 19 (COVID-19) Outbreak: Specific Precautions for Cancer Patients and Cancer Care Providers to Prevent Spread.” Asian Pacific Journal of Cancer Prevention 21 (2020): 569-573. doi:10.31557/APJCP.2020.21.3.569
- Liang W, Guan W, Chen R, et al. “Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China.” Lancet Oncol 21 (2020): 335-337. doi:10.1016/S1470-2045(20)30096-6
- Al-Shamsi, Humaid O., et al. “A Practical Approach to the Management of Cancer Patients During the Novel Coronavirus Disease 2019 (COVID-19) Pandemic: An International Collaborative Group.” The Oncologist 25 (2020): 936-945. http://dx.doi.org/10.1634/theoncologist.2020-0213
- “Coronavirus (COVID-19) Precautions.” mdanderson.org, https://www.mdanderson.org/patients-family/becoming-our-patient/planning-for-care/coronavirus-protections.html. Accessed 23 July 2020.
- Deb, Bijayeeta, Hemal Shah, and Suchi Goel. “Current global vaccine and drug efforts against COVID-19: Pros and cons of bypassing animal trials.” J Biosci 82 (2020): 1-10. doi:10.1007/s12038-020-00053-2
- Zhang, L. et al. “Clinical characteristics of COVID-19-infected cancer patients: a retrospective case study in three hospitals within Wuhan, China.” Annals of Oncology 31 (2020): 894-901. https://doi.org/10.1016/j.annonc.2020.03.296
- Pastick, Katelyn A., et al. “Review: Hydroxychloroquine and Chloroquine for Treatment of SARS-CoV-2 (COVID-19).” Open Forum Infectious Diseases (2020): 1-9. doi:10.1093/ofid/ofaa130
- Kourie, Hampig Raphael, Roland Eid, Fady Haddad, et al. “The future of cancer research after COVID-19 pandemic: recession?” Future Oncology 16 (2020): 1493-1495. doi:10.2217/fon-2020-0397